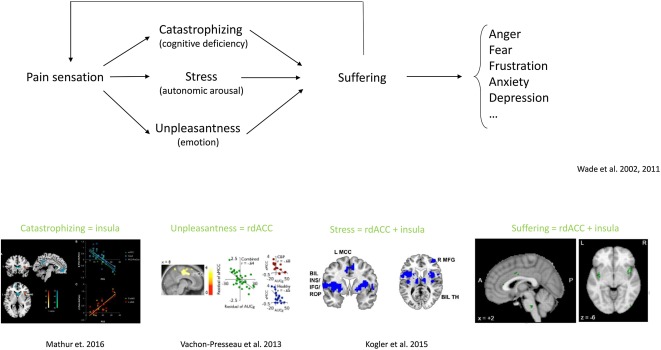
Pain sensation leads to suffering via a cognitive (insula), emotional (ACC) and autonomic (ACC plus insula) processing, and is expressed as anger, fear, frustration, anxiety and depression, leading to changes in behaviour and functional disability. – Science Direct
Psychosomatic pain and neurological pain represent two different concepts related to the perception and experience of pain, each with distinct underlying mechanisms.
An Overview of Neurological Pain:
-
- Definition: Neurological pain, also known as nociceptive pain or neuropathic pain, arises from damage or dysfunction in the nervous system.
- Causes: It can result from injuries, inflammation, or diseases affecting the peripheral or central nervous system. Examples include nerve compression (as in sciatica), diabetic neuropathy, and postherpetic neuralgia.
- Characteristics: Neurological pain is often described as shooting, burning, tingling, or electric shock-like. It may be associated with sensory abnormalities, such as hypersensitivity or numbness in the affected area.
- Diagnosis and Treatment: Diagnosis involves identifying the underlying neurological condition through clinical examination, imaging studies, and sometimes nerve conduction tests. Treatment may include medications targeting nerve pain, physical therapy, or interventions such as nerve blocks.
A Look at Psychosomatic Pain:
-
- Definition: Psychosomatic pain, also referred to as psychogenic pain or somatoform pain disorder, is pain that is influenced by psychological factors, such as emotions, stress, or mental health conditions.
- Causes: Psychosomatic pain does not have a clear physical cause or pathology; instead, it is thought to be related to the mind-body connection. It may be associated with psychological disorders like depression, anxiety, or somatization disorders.
- Characteristics: The pain experienced in psychosomatic conditions may not have a clear anatomical distribution or may move from one location to another. The severity of pain can be disproportionate to any physical findings.
- Diagnosis and Treatment: Diagnosis involves a thorough assessment of psychological factors contributing to the pain. Treatment typically involves a multidisciplinary approach, including psychotherapy, cognitive-behavioral therapy, and sometimes medications to address underlying psychological issues.
Pain and Suffering are Different
The sensation of pain(fullness) can lead to suffering via the associated feeling of unpleasantness and catastrophizing (Wade et al., 2011). The combination of the perceived unpleasantness and catastrophizing leads to suffering, which can express in different behaviors, including anger, fear, frustration, anxiety and depression (Wade et al., 2011; Wade and Hart, 2002; Bustan et al., 2015) as well as functional disability (Severeijns et al., 2001) (Fig. 4, Fig. 5). Suffering can thus be defined as an unpleasant experience associated with negative cognitive, emotional and autonomic impact leading to changes in behavior and functional disability.
Emerge Ketamine Can Help You Develop a Pain Management Plan
It’s important to note that these categories are not mutually exclusive, and there can be overlap between neurological and psychosomatic factors in pain experiences. The biopsychosocial model of pain recognizes the interplay between biological, psychological, and social factors in the perception and experience of pain. As a result, a comprehensive approach to pain management may involve addressing both the physical and psychological aspects of pain. A healthcare professional at Emerge Ketamine can help determine the most appropriate diagnostic and treatment strategies based on an individual’s specific situation.
References:
Dirk De Ridder, Divya Adhia, Sven Vanneste, The anatomy of pain and suffering in the brain and its clinical implications,
Neuroscience & Biobehavioral Reviews,
Volume 130,
2021,
Pages 125-146,
ISSN 0149-7634,
https://doi.org/10.1016/j.neubiorev.2021.08.013.
(https://www.sciencedirect.com/science/article/pii/S0149763421003560)

