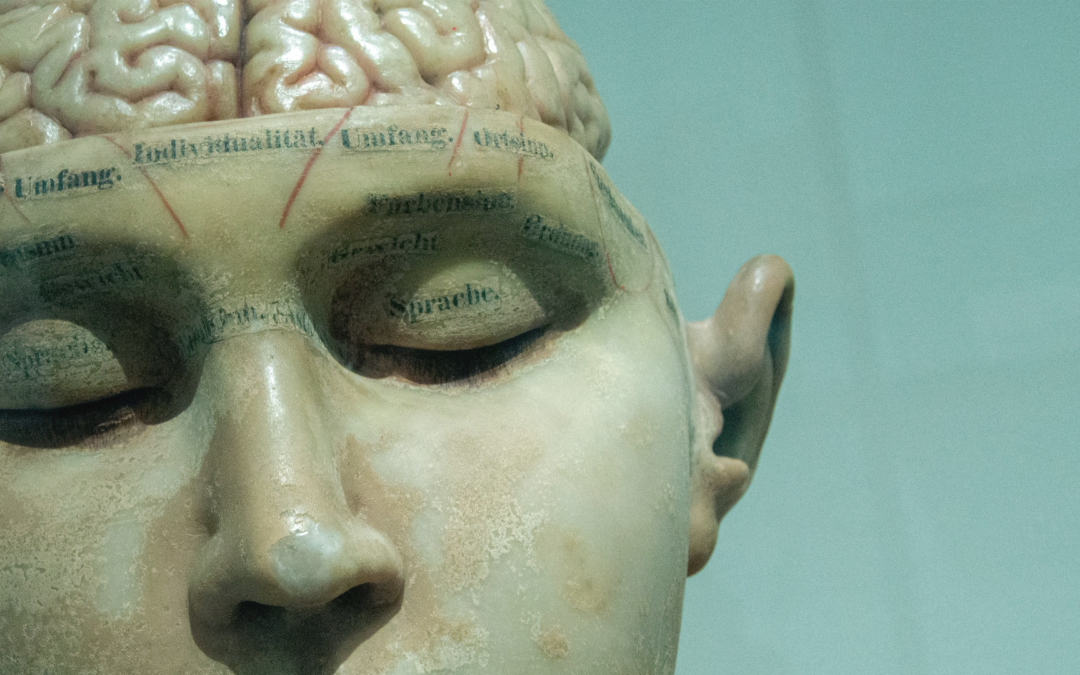
How does ketamine affect the brain? Originally developed as a surgical anesthetic, clinicians now study and use ketamine to treat various mental health conditions. This article explores the effects of ketamine on the human brain—how it influences mood, cognition, and neural activity—and why it has become such a powerful tool in psychiatric treatment.
What is Ketamine?
Researchers initially developed ketamine as an anesthetic. However, the drug’s uses have since expanded to treat a wide variety of conditions, including:
Ketamine is especially effective for people who haven’t responded to traditional treatments. It works rapidly, making it a valuable option for those experiencing suicidal thoughts or severe depression.
Ketamine’s Effects on Glutamate
Understanding how ketamine impacts glutamate pathways is key to understanding its brain effects. Glutamate is the brain’s main excitatory neurotransmitter. It helps nerve cells send signals that influence learning, memory, and pain perception.
Ketamine blocks NMDA receptors, which normally respond to glutamate. This reduces glutamate signaling, relieving pain and causing anesthesia at high doses. In chronic pain cases, this mechanism prevents amplified pain signals—one reason why ketamine is used to treat conditions like CRPS.
Ketamine and Glutamate Signaling
While ketamine dampens activity in some brain areas, it increases it in others. This paradox happens because ketamine disables inhibitory interneurons—cells that normally prevent others from firing. With these “off-switches” turned off, certain brain areas, like the prefrontal cortex (PFC), become more active.
This matters because the PFC helps regulate emotion. People with depression often show underactivity in this region. By reactivating it, ketamine may improve mood and reduce depressive symptoms.
Ketamine also enhances synaptic plasticity—your brain’s ability to adapt and form new connections. It boosts levels of BDNF, a protein that supports neuron growth. Additionally, it activates the mTOR pathway, which helps build proteins essential for creating new synapses. These mechanisms may help reverse damage caused by chronic stress or mental illness.
How Ketamine Alters Brainwaves
Brainwaves reflect how neurons communicate. EEG studies show that high doses of ketamine increase delta waves—associated with deep sleep. At low doses, ketamine raises gamma waves, which are linked to problem-solving, meditation, and heightened focus. These brainwave changes may explain some of ketamine’s antidepressant effects.
An EEG study found that high doses of ketamine increase delta waves—slow brainwaves linked to deep sleep and unconsciousness. On the other hand, low doses of ketamine increase gamma waves, which have the highest frequency and are associated with deep concentration, states of meditation, and problem-solving.
The research team suggested that ketamine’s ability to increase gamma waves may help explain its benefits in treating depression.
Ketamine Interaction with Dopamine
Dopamine is a neurotransmitter associated with pleasure, reward, and motivation. Ketamine can boost dopamine levels in the brain, explaining its ability to rapidly improve mood. Ketamine may also improve long-term connectivity between the PFC and the VTA, a key dopamine-producing region.
While ketamine’s effect on dopamine can benefit mood disorders, it also contributes to the drug’s addictive potential. Dopamine can reinforce people’s desire to seek out ketamine, leading to drug craving. With ongoing use, dopamine function can decline, requiring higher doses to feel the same effects.
Ketamine and Functional Connectivity
Functional connectivity (FC) is how different regions of the brain interact and work together. Brain scan experiments show that ketamine affects FC across areas of the brain, including:
Decreased activation of the default mode network (DMN): The DMN is a group of brain regions that becomes active when a person is not focused on a specific task, such as during rest or self-reflection. It is closely linked to one’s sense of self, to rumination–repetitive, often negative thought patterns–and overactivity has been associated with mood disorders. Ketamine can interrupt DMN activity, potentially helping people “break free” from harmful thought cycles.
Increased fronto-limbic coupling: The frontal cortex and limbic system are two key brain areas involved in emotion and decision-making. The frontal cortex helps with regulate emotional responses while the limbic system processes strong emotions. In mood disorders, the connection between these regions often becomes weaker or dysregulated, making it harder for people to manage negative emotions. However, by improving communication between these brain areas, ketamine may help support more effective mood regulation.
Final Words
While we continue learning more about how ketamine affects the brain, early studies provide valuable insight into its short-term effects and long-term potential. Researchers have made progress in studying ketamine’s brain effects, but its long-term impact remains unclear. Most studies focus on short-term outcomes, and there are open questions about how repeated treatments may affect the brain over months or years.
Future studies are needed to clarify ketamine’s risks, benefits, and long-term effects. As studies continue, the hope is to refine how ketamine is used—making it safer, more effective, and better suited to individual needs.